Avoid Surgery with Ultrasound Guided Ablations. We usually achieve excellent results with minimal complications
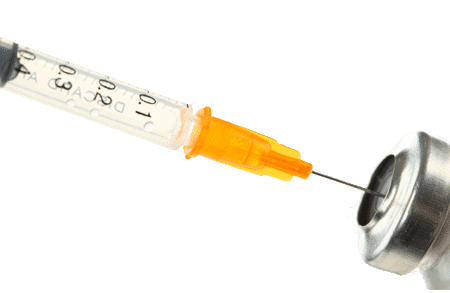
Ultrasound guided non-surgical procedures are the treatment of choice to cure Morton’s neuroma. We use ultrasound guidance for all our procedures and this allows us to visualize the needle tip when administering the treatment, confirming proper needle placement. Seeing the needle tip results in a higher degree of success and the prevention of injury to other local tissues. Furthermore, the use of ultrasound can help in the diagnosis of other local pathology, e.g. synovitis, bursitis or tendon pathology.
It is very common for conservative treatments and corticosteroid injections not to help in treating your Morton’s neuroma. Then more invasive treatment is warranted. Depending on your other medical conditions and an assessment by our one of our doctors, we perform one of these three ultrasound guided ablations:
If done by a specialist physician who is experienced in doing these procedures and done under ultrasound guidance, the above three procedures should be equally as effective, with success rates above 85%. To read the medical studies that show the effectiveness of these procedures for the treatment of Morton’s neuroma click here.
So which one is best for you? When you come, one of our doctors will do a full clinical assessment of you including a review of your past tests, a full examination of your feet, and an ultrasound guided local anesthetic diagnostic injection. This diagnostic injection is considered the gold standard for the diagnosis of Morton’s neuroma and gives us a good indication as to whether our ablation procedures will be successful.
At the time of your clinical evaluation, we will give you our recommendation as to which ablation procedure we feel is best for you.

Ultrasound guided radiofrequency ablation is a sophisticated, minimally invasive procedure that is associated with high patient satisfaction scores and long term pain relief for Morton’s neuroma. It is a procedure that uses high frequency radio waves to heat the sensory nerve that is affected in Morton’s neuroma to 90 degrees Celsius.
At this temperature the heat breaks down proteins preventing the nerve fibers from transmitting pain. The nerve is destroyed and the pain from that area is not transmitted any further. In addition, radiofrequency ablation may cause the creation of new blood vessels speeding up the healing process.
Radiofrequency ablation has been used in medicine for many years, particularly in the case of abnormal heart rhythms and back pain. The use in Morton’s neuroma is a relatively recent development. The procedure is minimally invasive and at our center these procedures are performed under local anesthetic with ultrasound guidance to ensure correct positioning.
It is a mostly painless procedure and you are likely to only feel pain when the local anesthetic is injected into the foot. On the day of the procedure, the area is anesthetized with local anesthetic. After it has taken effect, a very small puncture is made over the painful area. The radiofrequency needle is introduced and an ultrasound is used to guide the positioning of the needle.
Once the needle is in the correct position, an electrode is placed through the needle and the tip of the electrode is heated and repeated according to protocol. The site is covered with a bandage and patient is advised to reduce activity, ice and elevate the foot. The bandage can be removed the following day and patient can cover the area with a regular Band-Aid. You should keep the injection site clean and dry for at least 24 hours. Reduced activity can be resumed within one or two days of the procedure and any pain that occurs is usually managed with an NSAID or Tylenol. High impact activities on the ball of the foot should be avoided for a week or so. You can drive home on the day of the procedure.
Side effects are not generally seen with this procedure, but a few are a possibility. Infections are rare, as is abscess formation at the puncture site. You may develop bruising that can be painful. Numbness or a lack of feeling in around the incision area can also happen, but this side effect is rare.
You may experience relief from this procedure within a week or two, but frequently it takes a longer period of time to heal completely. If there is still pain at eight weeks, the procedure can be performed again.
Most patients find that after two ultrasound guided radiofrequency ablations their pain has decreased significantly. If, in the very rare case, ultrasound guided radiofrequency ablation has little effect it may be time to look at a different ultrasound guided ablation procedure.
To read the medical studies that show the effectiveness of radiofrequency ablation for Morton’s neuroma click here.


Ultrasound guided cryosurgery (also known as cryoablation) is similar to radiofrequency ablation in that it causes carefully targeted injury to destroy nerves to interrupt the pain. While radiofrequency ablation uses radio waves to create heat and break down nerves, cryosurgery uses cold/ice instead, using medical-grade nitrous oxide to generate extremely cold temperature to selectively destroy neuroma tissue.
It has been used for many years to relieve the pain of various nerve pathologies, including Morton’s neuroma. We use ultrasound guidance to increase the effectiveness of this treatment by ensuring the correct placement of the probe tip.
It is a mostly painless procedure and you are likely to only feel pain when the local anesthetic is injected into the foot. On the day of the procedure, the area is anesthetized with local anesthetic. After this has taken effect, a very small incision is made over the painful area. The cryoprobe is introduced and an ultrasound is used to guide the positioning of the probe. Once in the correct position, freezing and repeated according to protocol.
The site is covered with compression bandage and patient is advised to reduce activity, ice and elevate for the remainder of the day. The bandage can be removed the following day and patient can cover the area with a regular Band-Aid.
You should keep the injection site clean and dry for at least 24 hours. Normal activity can be resumed within one or two days of the procedure and any pain that occurs is managed with a NSAID or Tylenol. Pain continues to reduce over a two-week period; if at the end of a four-week period the reduction is not sufficient, the procedure can be repeated.
The cyroprobe used in cryotherapy creates a 6-8mm ice ball at its tip that reaches temperatures of -70 degrees Celsius, which freezes the Morton’s neuroma, prevents nerve transmission and decreases pain. This ball of ice degenerates the outer sheath of the nerve (demyelinazation) and destroys part of the nerve (Wallerian-like degeneration). The ice ball destroys about one cm of the nerve, which regenerates back at between one to three millimeters per day; therefore the axon or nerve regeneration should be complete within several weeks. It appears long lasting pain relief is due to the reduction of both nerve swelling and nerve sheath scarring.
You should keep the injection site clean and dry for at least 24 hours. Reduced activity can be resumed within one or two days of the procedure and any pain that occurs is usually managed with an NSAID or Tylenol. High impact activities on the ball of the foot should be avoided for a week or so. You can drive home on the day of the procedure.
In the past, the cryoablation was blindly applied to the area, but recent advances in ultrasound technology has allowed for careful placement of the probe and therefore better results. Pain relief is more complete and decreases the need for further procedures.
Cryoablation (or cryosurgery) differs from radiofrequency ablation in that the pain relief from cryoablation can be a little sooner than radio frequency which can sometimes take up to two months to demonstrate effective pain control. The use of cold also decreases the risk of a further neuroma that can sometimes occur after surgical intervention. When very little or no pain relief occurs, it is frequently because of dense scar tissue related to previous Morton’s neuroma treatments in the foot. In these cases inserting the cryoprobe through the underside (plantar) aspect of the foot can often overcome this problem.
However, in some cases, cryosurgery can also take up to 2-3 months for full pain relief to be achieved. Side effects are rare with this procedure and may include bruising, infection or frostbite at the area of insertion. You may also feel a small lump in your foot where the procedure was performed. This generally goes away within 3 to 6 months and does not cause pain.
Virtually all Morton’s neuroma patients who have had cryoablation or cryosurgery for Morton’s neuroma have maintained full motor function with no greater loss of sensation than prior to the procedure. If patients are unlucky enough to experience a return of Morton’s neuroma symptoms the cryoablation procedure can simply be repeated or other non-surgical treatments can be performed.
Most patients find that after two (or three) cryoablations their pain has decreased significantly. If, in the very rare case, ultrasound guided cryoablation has little effect it may be time to look at a different ultrasound guided ablation procedure.
To read the medical studies that show the effectiveness of cryoablation for Morton’s neuroma click here.
Neurolytic injections inject a mixture of a sclerosing agent (usually concentrated alcohol) and local anesthetic directly into the Morton’s neuroma in order to eliminate or significantly diminish the ability of the nerve to transmit pain signals, thereby reducing pain sensation.
An experienced practitioner should do the procedure under ultrasound guidance. The use of an ultrasound to guide needle placement is especially important when using high concentrations of neurolytic agents to ensure that the neurolytic agent does not leak from the immediate area surrounding the Morton’s neuroma. If a leak occurs, the neurolytic agent can damage the surrounding structures.
The affected area is anesthetized with local anesthetic. Once this has taken effect, a mixture of the neurolytic agent and local anesthetic is injected to the Morton’s neuroma using ultrasound guidance to ensure proper needle placement. The procedure is minimally invasive and at our center, is performed by one of our specialists who specialize in these types of ultrasound-guided procedures.
This injection may shrink the neuroma but that is unlikely – it just kills it and usually results in very little complications aside for some minor numbness which is less than the size of a penny in the webspace. The numbness lasts about 6 months.
After the procedure, the injection site is covered with a small Band-Aid for protection. Patients wait 15 -30 minutes following the injection, and then they can carefully move around the office. Morton’s neuroma patients can obtain pain relief within 1 -2 weeks following the procedure. Patients to return to normal activities the following day. With this type of injection, follow up appointments are vital. If significant pain relief is achieved but pain still persists, the procedure can be repeated after a 4 week interval.
Most patients find that after two ultrasound guided neurolytic injections their pain has decreased significantly. If, in the very rare case, the ultrasound guided neurolytic injection has little effect it may be time to look at a different ultrasound guided ablation procedures.
Rarely, the nerve can regrow and it may become irritating or painful again although if that occurs it’s usually after 6-8 years and then it requires a single repeat neurolytic injection.
When done by experienced practitioners, this procedure has few side effects but in rare cases, they can occur. First, non-target tissue is at risk for being damaged by the neurolytic agent resulting in the sloughing off of skin or possibly a non-healing wound. Second, the neuroma may grow back and cause the initial pain that prompted the procedure, but this occurs years later. Finally, numbness and tingling in the toes may be noted if other portions of the nerve become damaged.
To read the medical studies that show the effectiveness of neurolytic injections for Morton’s neuroma click here.
The second type of alcohol injection is a neurolytic alcohol injection done with much higher concentrations of alcohol. (We use more than 10 times the dose of the sclerosing injection.) In effect these injections deaden the neuroma and completely remove the neuroma’s ability to transmit pain and stop the neuroma from growing. Since these injections are done with much higher alcohol concentrations, they should always be done under Ultrasound guidance by clinicians who are highly experienced in doing these.
They are very effective and recent research shows that they have over 85% efficacy. We believe the efficacy of these is even higher when done by an experienced clinician under ultrasound guidance.
This is the “typical” alcohol sclerosing injection done by many podiatrists. This is usually done with a very low concentration of alcohol (usually around 4% alcohol) which is blindly injected into the neuroma and frequently repeated for four, five or six times.
We believe that this type of injection has little effect and only results in scar tissue growth and greater discomfort for the patient.
However for reasons we cannot understand, it is commonly done.
By providing us with your information you are consenting to the collection and use of your information in accordance with our Terms of Service and Privacy Policy.