Ultrasound guided cyrosurgery (also called cyroablation) is a minimally invasive technique that is used for the treatment of Morton’s neuroma. This procedure involves the use of extremely cold temperatures to freeze the neuroma nerve cells, which causes them to degenerate and stop transmitting pain signals. In other words, this stops you from feeling any pain and stops the neuroma from growing. Ultrasound guided cyrosurgery is ideally reserved for patients that have tried conservative remedies and wish to treat their Morton’s neuroma without surgery.
In United States alone over the last 10 years, more than 50,000 cryosurgeries for Morton’s neuroma have been performed with a success rate of over 80% (without any major acute or delayed complications). Ultrasound guided cryosurgery is a more recent innovation with generally higher success rates.
What should you know about the ultrasound guided cyrosurgery procedure?
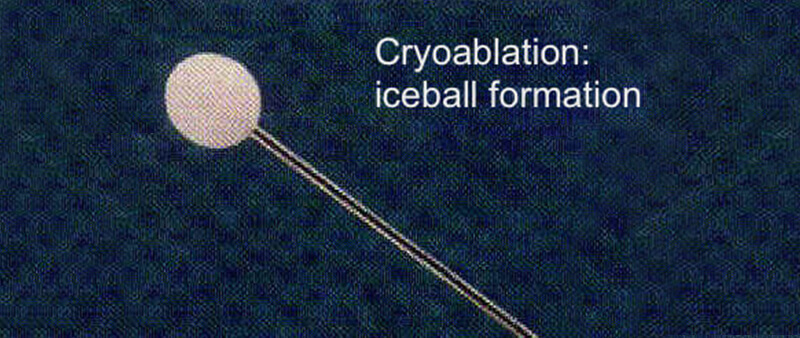
Ultrasound guided cyrosurgery is performed with the help of a specialized instrument (also referred to as the cryoprobe) used under ultrasound guidance. The cryoprobe is capable of delivering a temperature of about -50 to -70 degrees Celsius which creates an ice-ball (about 6-10mm in diameter). The cold temperatures from the ice-ball inhibit the circulation and supply of blood to the neuroma. This freezing temperature is sufficient to damage the blood vessels that supply the nerve sheath of the affected nerve (thereby leading to degeneration and demyelination of the nerve tissue) in a process known as Wallerian degeneration.
Ultrasound guided cryosurgery – Morton’s Neuroma
Ultrasound guided cryosurgery is superior to Morton’s neuroma surgery because:
What to expect after the ultrasound guided cyrosurgery procedure?
Ultrasound guided cyrosurgery is usually followed by mild localized pain and little to no bruising. In most cases, the pain and bruising disappears within 3-4 days post-procedure. Complete resolution of pain occurs within 2-4 weeks after the procedure.
According to a research study published in the Journal of Foot and Ankle Surgery(1), investigators reported the results of cryoablation for Morton’s neuroma. The study concluded that cryosurgery is at lease as effective as surgical intervention however, post-procedure disability scores and patient satisfactions scores are much higher in cryosurgery when compared to conventional surgical interventions.
Complications of cryosurgery:
Cryosurgery is a fairly safe procedure with a minimal risk of complications. Some complications have been reported such as:
The rate of complications is usually negligible if the procedure is performed by a provider well experienced in ultrasound guided cryosurgery.
Contraindications of cryosurgery for Morton’s neuroma:
Although Cryosurgery is an excellent procedure for the long term management of Morton’s neuroma; it may not be an appropriate option for some individuals. For example, individuals who are suffering from peripheral artery disease (advanced atherosclerosis) or compromised circulation are not ideal candidates for this procedure. This is mainly because exposure to cold temperature may aggravate the risk of nerve damage and vascular fibrosis in these subjects. Moreover, individuals with a history of Raynaud’s disease (or other autoimmune disorders) are also not ideal candidates for this procedure.
Morton’s neuroma is a chronic and debilitating condition that gradually compromises the quality of an individual’s life. Thankfully, there are several excellent non-surgical procedures that we offer to treat Morton’s neuroma and these interventional treatments result in long term pain relief and resolution of symptoms. Click here to see a list of the non-surgical Morton’s neuroma treatments we offer.
Cryosurgery for your Morton’s neuroma may a suitable procedure for you. You should discuss your treatment options with a provider who is well experienced with a range of non-surgical options to decide which is the best solution for you.
1. Caporusso, E. F., Fallat, L. M., & Savoy-Moore, R. (2002). Cryogenic neuroablation for the treatment of lower extremity neuromas. The Journal of foot and ankle surgery, 41(5), 286-290.
By providing us with your information you are consenting to the collection and use of your information in accordance with our Terms of Service and Privacy Policy.