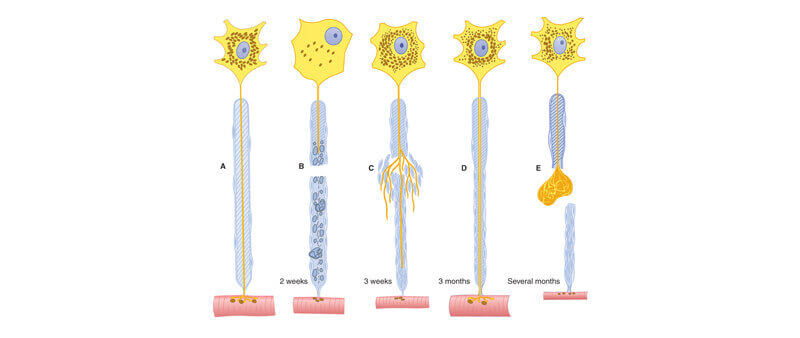
Every time you cut a peripheral nerve you always generate specific biochemical response called a “Wallerian degeneration.”
This reaction occurs every single time a nerve is cut. It is the body’s natural response to a cut nerve. In simple terms, Wallerian degeneration is a cascade of cell responses to the cut nerve that result in nerve regrowth. This nerve regrowth begins within 4 days after the nerve is cut. The normal physiological response of the body to a cut nerve in the foot is for the nerve to begin to regrow. In the case of a Morton’s neuroma removal (also known as a Morton’s neurectomy), this regrowth is the beginning of a stump neuroma.
The body’s natural reaction to a Morton’s neuroma surgery (Morton’s neurectomy) is to create a stump neuroma. In the case of a Morton’s neuroma surgery (neurectomy), a section of the Distal Plantar Nerve is removed and the body’s natural reaction to this injury is for the nerve ending to regrow. Therefore a stump neuroma develops as the budding nerve cells in the near section of the cut nerve trunk multiply and grow in a tangled disorganized fashion as they attempt to bridge the gap towards the other side of the cut nerve (i.e. part of Wallerian degeneration). The newly budding nerve cells tangle amongst themselves and become entrapped in scar tissue and can stick to neighboring structures, such as the metatarsophalangeal joint capsule, the bone surface (the periosteum of the metatarsal shaft), and nearby tendons, ligaments, and muscle. If the stump neuroma adheres to one of the adjacent metatarsal heads, it causes a lot of pain !
Surgeons have desperately tried various measures to prevent this Wallerian degeneration but they are fighting an uphill battle because they are trying to prevent the body’s normal response to a cut nerve. Many surgeons use steroid, alcohol or dilute phenol infiltration into the proximal nerve stump to attempt to decrease the chance of a post surgical stump neuroma forming but these have not been proven to help. Some surgeons cap the proximal nerve stump with silicone during the operation but this has also yielded inconsistent results and very often requires reoperation to remove the silicone cap and revise the surgery. Nowadays many surgeons try to bury the nerve ending in the adjacent muscle, a technically difficult solution which is also not fully effective.
In contrast, killing the nerve through the use of ultrasound guided cryoablation, ultrasound guided radiofrequency ablation or ultrasound guided neurolytic injections, does not illicit a Wallerian degeneration of the nerve. Even though the nerve dies, it goes through what is known as a “Wallerian-like degeneration” and not a true Wallerian degeneration. For a true Wallerian denegation to occur, the nerve must be cut or injured to such an extent that the nerve sheath is injured and the nerve fibers are separated. Ultrasound guided ablation procedures do not cut the nerve. So even though nerve goes through a degeneration process, the nerve sheath and the nerve fibers are still intact preventing the nerve regrowth that causes a stump neuroma.
It is this reason that an ablation procedure never causes a stump neuroma, while a surgical Morton’s neurectomy (which cuts and removes part of the nerve) always causes a stump neuroma unless the surgeon can do something to interfere with the body’s natural nerve healing process.
Ablation procedures can still fail, especially if they are not done under ultrasound guidance by experienced clinicians, but the ablation never results in a stump neuroma. Ablation procedures can rarely fail even when done by experienced clinicians under ultrasound guidance. If they do not produce the desired pain relief they can be easily repeated.
By providing us with your information you are consenting to the collection and use of your information in accordance with our Terms of Service and Privacy Policy.