These sound so similar. Whats the difference? How do you know if you have one and not the other?


Synovitis is inflammation of the tissues that line a joint causing increased fluid in the joint and even joint instability. In general Synovitis is commonly associated with specific diseases such as arthritis or gout, but may also be the result of overuse or trauma. Symptoms of synovitis may include redness, swelling, warmth, and pain with joint motion.
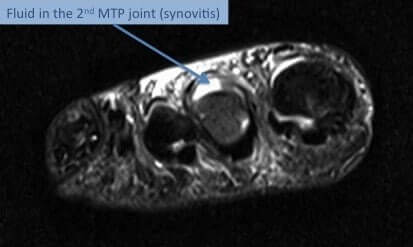
MTP synovitis frequently produces sharp aching pain that is most pronounced along the ball of the foot. The pain is usually suggestive of an ongoing disease process and usually involves the second metatarsophalangeal joint. The most common cause of MTP synovitis is repetitive stress on the metatarsophalangeal joint that results in persistent inflammation and resulting degeneration of tissues and ligaments that supports the base of toes. The stress is increased when the pressure on the ball of foot increases.
Common risk factors that may increase the risk of developing MTP synovitis are:
Some signs that are strongly suggestive of MTP synovitis are:

Ligaments surrounding the joint at the base of the toe form a “capsule,” which helps the joint to function properly. Capsulitis is a condition in which these ligaments have become inflamed.
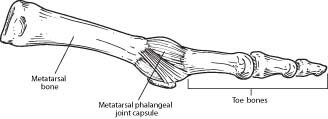
Although capsulitis can also occur in the joints of the third or fourth toes, it most commonly affects the second toe. This inflammation causes considerable discomfort and, if left untreated, can eventually lead to a weakening of surrounding ligaments that can cause dislocation of the toe.
Capsulitis is due to abnormal foot mechanics combined with repetitive foot motion that exerts pressure on the ball of foot to cause connective tissue degeneration. Poor foot dynamics or chronic stress can cause MTP capsulitis. Certain risk factors that may aggravate the risk of MTP capsulitis are:
Classic sign and symptoms that are suggestive of MTP capsulitis are:
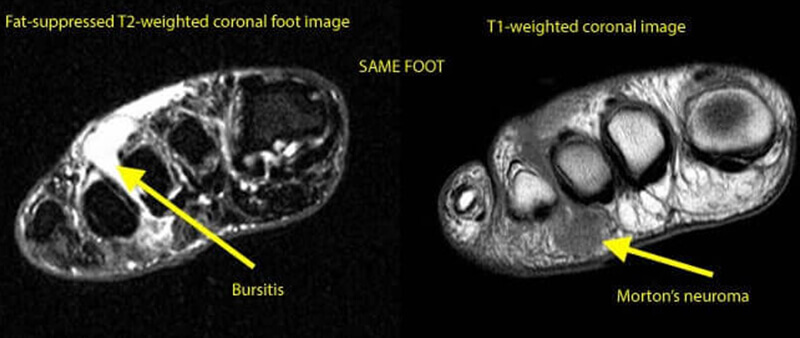
Bursitis is inflammation and a painful swelling of a small sac of fluid called a bursa. Bursae (plural of bursa) are fluid filled cushions that help absorb shock and lubricate areas where tendons, ligaments, skin, muscles, or bones rub against each other. People who repeat the same movement over and over or who put continued pressure on a joint in their jobs, sports, or daily activities have a greater chance of getting bursitis.
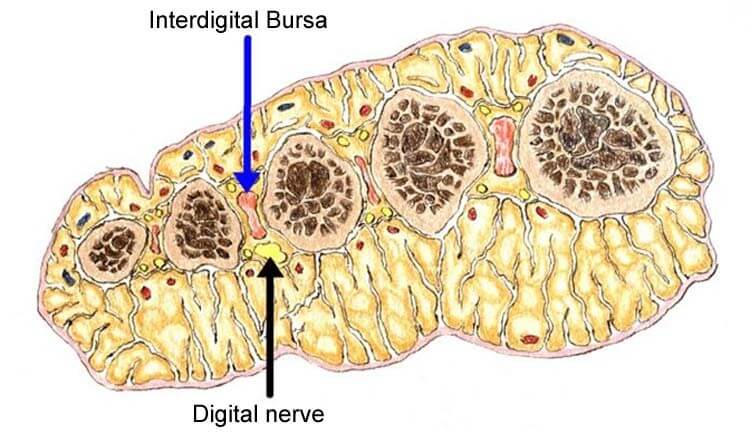
The anatomical location of MTP bursa is at the base of metatarsophalangeal joint. Any condition that causes over-riding of metatarsal bones can aggravate the risk of developing bursitis as a result of tissue compression in the region.
Many cases of Morton’s neuroma present with adjacent bursitis and in some cases it can be very hard to differentiate the true cause of pain. In most cases, painful MTP bursitis involves first MTP joint. A bunion together with pain around the MTP joint is suggestive of MTP bursitis.
Certain risk factors that may aggravate the risk of MTP bursitis:
The classic presentation of MTP bursitis is:
Untreated cases of large MTP bursitis can lead to rheumatoid arthritis and related degenerative types of joint dysfunction.
Inflammatory lesions of MTP joint (synovitis, capsulitis, bursitis) usually responds to conservative therapies and surgery is not usually required in most cases. Most common interventions are:
References:
By providing us with your information you are consenting to the collection and use of your information in accordance with our Terms of Service and Privacy Policy.