Morton’s neuroma is a common foot condition that is marked by onset of moderate to severe foot pain, abnormal sensations and other signs of inflammation. Is is caused by the compression of interdigital nerves due to persistent pressure and inflammatory damage to the fibrous tissues that surrounds the nerve fibers. The clinical diagnosis of Morton’s neuroma is a little tricky. This is mainly because, a number of foot pathologies may mimic Morton’s neuroma in symptomatology and presentation. For a discussion of conditions that can mimic Morton’s neuroma, click here.

Diagnosis of Morton’s neuroma and nerve entrapment syndromes
A number of nerve entrapment syndromes can mimic Morton’s neuroma.
Other common conditions that are confused with Morton’s neuroma in terms of symptomatology are hammertoe, bursitis, ganglion cysts, arthritis and stress fractures. It is highly recommended to see a practitioner who has significant experience with Morton’s neuroma to ensure the correct diagnosis.
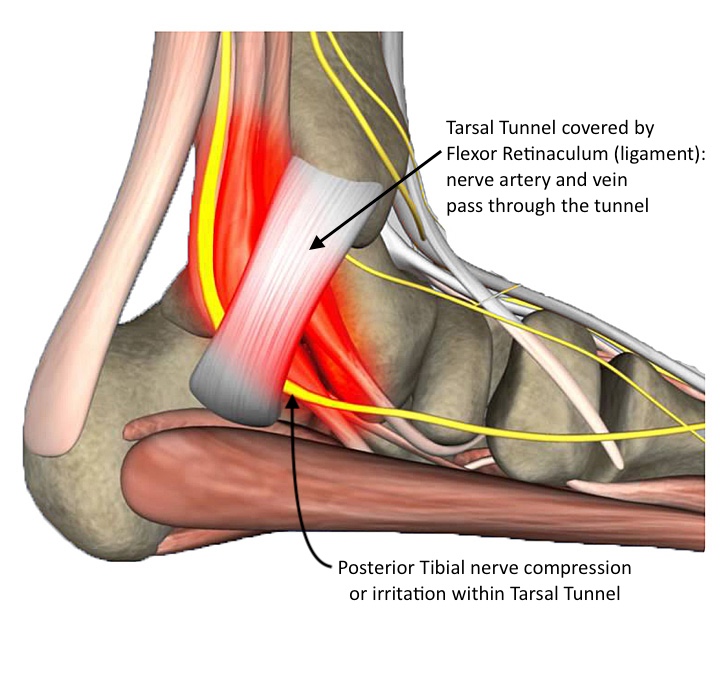
Tarsal Tunnel Syndrome vs. Morton’s neuroma:
According to a new study reported in the journal Foot and Ankle Clinics(1), investigators often confuse Morton’s neuroma diagnosis with tarsal tunnel syndrome on accounts of the similarities in the clinical presentation. This can be explained by the anatomical variations of tibial nerve in different individuals. Study reported in Foot & Ankle International(2) journal reports that in some individuals, the Tarsal nerve splits behind the laciniate ligament; while in others, the nerve gives off several branches near medial-malleolar-calcaneal axis(2). In simple words, this variability in anatomy results in entrapment or compression of tibial nerve that may produce variable symptoms. This can make it more challenging to clinically differentiate Tarsal Tunnel Syndrome from other foot conditions like plantar fasciitis and Morton’s neuroma.
Classic symptoms of Tarsal tunnel syndrome are:
Most Morton’s neuroma patients presents with similar symptoms (although not foot swelling). For a discussion on the diagnosis of Morton’s neuroma, click here.
The factors that are proven to aggravate the risk of tarsal tunnel syndrome are;
In simple words, any condition that aggravates the pressure on the tibial nerve or compress the contents of tarsal tunnel can lead to tarsal tunnel syndrome (such as flat arches).
How to Diagnose and Manage Tarsal Tunnel Syndrome?
Accurate and early diagnosis of nerve entrapment syndromes helps in adopting less invasive treatment options. Tarsal tunnel syndrome can be differentiated from Morton’s neuroma by:
A decline in electrical conductivity suggests entrapped nerve. However, it is imperative to keep in mind that the electromyography (EMG) study is not always reliable, as decreased conductivity is also observed in arthritis.
Performing Tinel’s Test
A positive tinel’s sign for tarsal tunnel syndrome is characterized by onset of pin and needle sensation along the medial aspect of the foot when the examiner taps on the tarsal tunnel/ behind the medial malleolus (or medial prominence of the ankle).
Clinicians can also perform Tinel’s sign for Morton’s neuroma diagnosis (by tapping on the third and fourth metatarsal space) to reproduce the symptoms of pain and discomfort.
Treatment
Provision of conservative care with the help of an arch support.
Surgical management options includes; releasing the lacinate ligament and decompression of the posterior tibial nerve by surgical manipulation. Generally the recovery time varies from 4 to 18 months and the outcome depends on the degree of entrapment.
References:
By providing us with your information you are consenting to the collection and use of your information in accordance with our Terms of Service and Privacy Policy.