If I have have symptoms that suggest Morton’s neuroma, is an ultrasound needed? Is an Magnetic Resonance Image (MRI) needed?
In the continuing discussion of ultrasound versus MRI for Morton’s neuroma, it looks like ultrasound is the winner. In a recent study(1), both ultrasound (90%) and MRI (93%) had similar high sensitivity rates (ultrasound (90%) and MRI (93%).) That means they were both similarly likely to detect a Morton’s neuroma.
However, MRI had a relatively lower specificity: MRI specificity was 68% versus ultrasound which was 88% in the detection of Morton’s neuroma. In other words MRI can lead to more false negatives – giving you a false negative diagnosis.
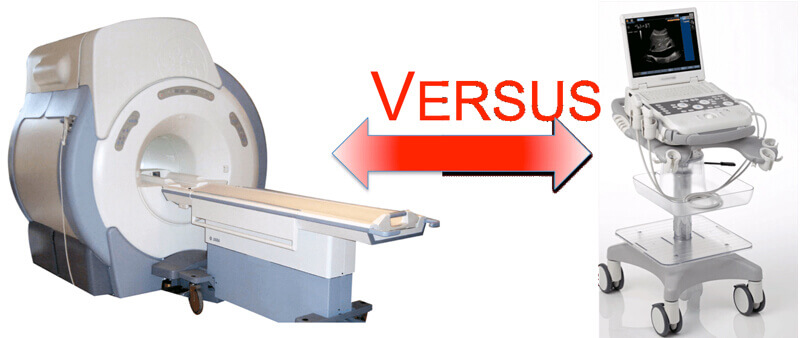
Comparing the two diagnostic tests, ultrasound had a higher positive likelihood ratio than MRI (2.77 versus 1.89) and lower negative likelihood ratio (0.16 versus 0.19)(1).
Another conclusion from the studies is that MRI is really not needed unless another diagnosis is in question and needs to be excluded.
The most important conclusion(2) is that Morton’s neuroma is a clinical diagnosis, because MRI and ultrasound both have false negatives and false positives (which are not that uncommon.) In other words, seeing a Morton’s neuroma on MRI or ultrasound does not mean that your foot pain is due to Morton’s neuroma and conversely a negative MRI or ultrasound doesn’t mean that you don’t have a Morton’s neuroma.
Remember always see a provider who has experience with diagnosing Morton’s neuroma. If in doubt, a diagnostic local anesthetic injection is the best diagnostic test especially when done under ultrasound guidance by an experienced provider.
By providing us with your information you are consenting to the collection and use of your information in accordance with our Terms of Service and Privacy Policy.