One of the complications of Morton’s neuroma surgery and Morton’s neuroma corticosteroid injections is Fat Pad Atrophy. It causes significant foot pain and metatarsalgia.
Fat pad atrophy is a common yet underdiagnosed condition that can cause significant discomfort in the heel or ball of the foot. Often mistaken for other foot ailments, it involves the thinning of the protective fat layer under the foot, leading to pain and sensitivity, especially on hard surfaces.
In many cases, the loss is due to the result of cortisone injections. Many people suffering with Morton’s neuroma foot pain or Metatarsalgia receive cortisone injections for the temporary relief of pain. However, these corticosteroid injections have a significant risk of resulting in fat pad atrophy, especially if they have been repeated a few times.
We can treat Fat Pad Atrophy with your own fat extracted from a mini liposuction done on your abdomen or buttocks, then processed and injected into your feet in an orthobiologic treatment.
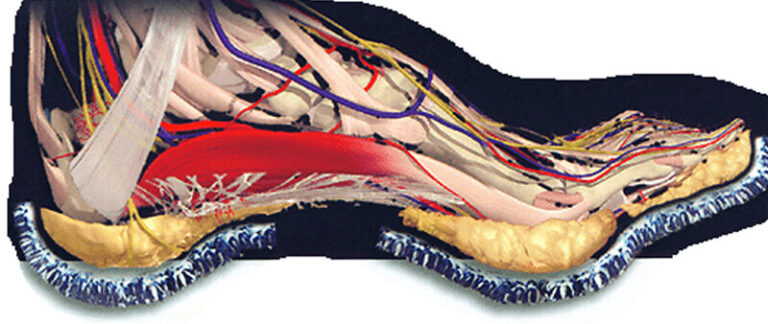
Fat pad atrophy occurs when the protective cushion of fat beneath your heel or ball of the foot begins to thin out. This thinning exposes the underlying bones to stress and impact, leading to discomfort and potential damage.
Several factors contribute to the development of fat pad atrophy, including:
Understanding these causes can help you adopt preventive measures. Learn more about prevention.
Fat pad atrophy doesn’t affect everyone equally. Let’s explore the groups that are most at risk:
As part of the natural aging process, the fat pads in the feet tend to shrink and lose their elasticity. This makes individuals over 50 more vulnerable to the condition, especially if they have an active lifestyle or spend a lot of time on their feet.
Corticosteroid injections are a common early treatment for metatarsalgia and Morton’s neuroma. These injections are frequently repeated. Repeated Cortisone injections result in a breakdown of fat pad tissue which does not repair or reverse.
People who engage in sports like running, basketball, or dance place repetitive stress on their feet. Over time, this constant impact wears down the protective fat layers, leading to pain and discomfort.
Shoes that lack proper cushioning or force the foot into unnatural positions, such as high heels or narrow-toed shoes, can compress the fat pads and lead to their breakdown. Wearing supportive footwear is crucial for prevention.
Certain health conditions increase the likelihood of fat pad atrophy, including:
Structural issues like flat feet, high arches, or bunions can disrupt the even distribution of pressure across the foot, putting excessive strain on specific areas and increasing the risk of fat pad thinning.
By understanding these risk factors, you can take proactive steps to protect your foot health.
We offer a range of non-surgical and surgical treatments to manage fat pad atrophy effectively.
Preventing fat pad atrophy involves making lifestyle and footwear adjustments to reduce stress on the feet:
Learn more about how to protect your feet.
Recent studies highlight the effectiveness of fat pad augmentation in the treatment of Fat Pad Atrophy.
Lipofilling for functional reconstruction of the sole of the foot. Nicoletti G; et al; Foot (Edinb). 2014 Mar;24(1):21-7. doi: 10.1016/j.foot.2014.02.003. Epub 2014 Mar 6. Link to Article
Autologous Fat Grafting for Pedal Fat Pad Atrophy: A Prospective Randomized Clinical Trial; GusenoffJ et al; Reconstr Surg. 2016 Nov;138(5):1099-1108. Link to Article
Fat Grafting for Pedal Fat Pad Atrophy in a 2-Year, Prospective, Randomized, Crossover, Single-Center Clinical Trial; Minteer et al; Plast Reconstr Surg. 2018 Dec;142(6):862e-871e. Link to Article
A: Fat Pad Augmentation. We can treat Fat Pad Atrophy with your own fat extracted from a mini liposuction done on your abdomen or buttocks, then processed and injected into your feet in an orthobiologic treatment.
A: No, we only do one for the time. If you need both feet then then we do your second for at least one month after the 1st foot.
A: Walk only as needed for the first three days. Using crutches is preferable. Within the next two weeks, you can walk but keep your foot elevated whenever you can.
For the first 4 to 6 weeks:
A: You should notice a change within the first six months, and this will continue to improve for two years thereafter.
A: While the condition does not reverse, symptoms can be managed in the short term with proper care and custom orthotics.
A: Fat pad atrophy causes pain under the heel, while plantar fasciitis typically causes pain in the arch and heel, especially after resting. Sometimes it can be very difficult to distinguish between the two and you should seek a provider who has a lot of experience in dealing with these two conditions to make an accurate diagnosis.
A: Surgery is rarely required and is usually reserved for very severe cases.
A: Shoes with thick, cushioned soles and proper arch support are ideal.
Have more questions? Contact us.
By providing us with your information you are consenting to the collection and use of your information in accordance with our Terms of Service and Privacy Policy.